The temperature had finally settled down to a mild -15 degrees in Ottawa when Louise Crandall and I sat down to discuss the new Supreme Court Ruling over Physician Assisted Suicide. Louise has worked for three health organizations including the Victorian Order of Nurses (VON), and has a positive opinion on the new ruling. She is currently volunteering at HelpAge Canada, an international organization that provides assistance to destitute seniors.
We are fortunate to be even discussing this. People in most developing countries do not have the luxury of thinking about these options. They have limited access to palliative care or pain medications. Families are left to provide in whatever way they can. There is no such luxury as end-of-life care.
Both my parents died at home in India. My father chose to go back to his village. He died in peace and away from over-crowded hospitals. I did not think much about this at the time. It was simply a sad farewell.
……………………………..
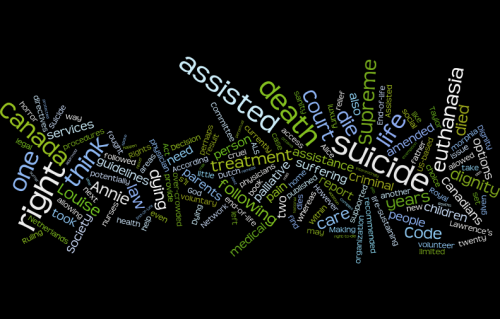
There are many complex procedures included under “assisted dying” – an umbrella term used to cover one or all of the following options:
• Withdrawal of potentially life-sustaining treatment
• Withholding of potentially life-sustaining treatment
• Providing life shortening symptom relief
• Palliative or terminal sedation
• Assisted suicide
• Voluntary euthanasia
• Advance directives that explicitly outline what treatment the person does or not want at end-of-life.
Louise’s father believed in allowing oneself to die with dignity. He spoke of an organization based on the ‘Right to Die Movement’ where directives were given on how to commit suicide. He had a book on the subject, but in the end he had an unpleasant death in hospital.
I looked up the US-based Final Exit Network formed in 2004 following the merger of End-of-life Choices (formerly known as the Hemlock Society) and Compassion in Dying. The website states that the Network has developed a system of volunteer guidelines to help dying people who request assistance.
http://www.finalexit.org/chronology_right-to-die_events.html
According to the Network’s Chronology of Rights, it was in 1998 that Oregon’s Death with Dignity Act was implemented. The Swiss Association, DIGNITAS, was founded in the same year and accepted members from abroad. In 2002, the Dutch law allowing volunteer euthanasia and physician-assisted suicide took effect although the procedures codified in the law had been a convention of the Dutch medical community for over 20 years (http://en.wikipedia.org/wiki/Euthanasia_in_the_Netherlands)
In 2008, the State of Washington approved a law similar to the one in Oregon. Montana followed in 2009, and in 2012, the world’s first mobile euthanasia unit was set up in the Netherlands.
……………………………
In Canada, an open debate followed by an amendment to the Criminal Code is desperately needed. Between 1991 and 2010, there were at least six private member bills presented seeking to decriminalize assisted suicide. However, none of these was passed. In 2011, the Royal Society of Canada published a report, End-of-life Decision Making, stating that “there is a pressing need for a set of national consensus guidelines” (P.28)
https://rsc-src.ca/sites/default/files/pdf/RSCEndofLifeReport2011_EN_Formatted_FINAL.pdf
In 2012, The Quebec National Assembly’s Select Committee published its report, Dying with Dignity, recommending that “the Collège des médecins du Québec amend its Code of Ethics so that physicians may provide medical aid in dying accordance with the criteria provided by law while confirming their right to conscientious objection and their obligation, in such a case, to refer their patient to another physician.” (P.101) The Committee also recommended that the Act respecting health services and social services be amended “to recognize the right of any individual to receive palliative care when warranted by his medical condition.” (P.98)
http://www.dyingwithdignity.ca/database/files/library/Quebec_death_with_dignity_report.pdf
According to the 2011 Royal Society of Canada’s End-of-Life Decision Making report, Canadians are living longer than ever before, and within the next twenty years, the population of people over 65 will double. Location of death is becoming increasingly important. Overwhelming evidence indicates that Canadians wish to die at home even though the vast majority currently dies in institutions. It is estimated that 95% of deaths would benefit from palliative care, yet 70% of Canadians lack access to adequate services due to uneven distribution of programs. Populations in remote or rural areas, for example, have very limited resources, while those in over-crowded urban areas have to face long wait times. In addition, there are few financial supports available for families and caretakers.
Another issue is regarding those who would be willing to engage in assisted suicide. Interestingly, whereas 55% of physicians have indicated their unwillingness to perform voluntary euthanasia or assisted suicide, 73% of nurses and social workers have said that the criminal code should be amended to permit voluntary euthanasia. They have also stated that nurses should be allowed to practice this. (PP. 11-24)
Louise suggested that perhaps there is an argument for leaving the field unregulated. Physicians can already decide on when to withdraw or withhold live-saving treatment. It is perhaps better not to have restrictive laws. But when one thinks of Dr. Kevorkian or Robert Latimer, both convicted of second-degree murder, one can say with conviction that we need clearer guidelines.
One’s point of view becomes more transparent when young children are in pain. The 2011 Report refers to a recent US-based survey of parents of children who had died of cancer. It was found that 50% of parents supported hastening death, whereas 94% supported intensive pain management.
…………………….
I think of instances in the past when I was forced to question my own position around assisted death. I remember reading the second-last chapter, “Release,” from D.H. Lawrence’s famous 1913 novel, Sons and Lovers.
Annie and Paul are in heart-wrenching agony while watching their beloved mother, Mrs. Morel, die of a large tumor she had not disclosed to anyone:
’She’ll live over Christmas,’ said Annie. They were both full of horror.
‘She won’t,’ he replied grimly. ‘I s’ll give her morphia.’…..
‘Ay – do!’ said Annie…..
That evening he got all the morphia pills there were and took them downstairs. Carefully he crushed them to powder.
‘What are you doing?’ said Annie.
‘I s’ll put ‘em in her night milk.
Then they both laughed together like two conspiring children. On top of all their horror flickered this little sanity.
I think of my school where life was said to be a gift from God – not ours to take. But interference with death should be equally unethical. What gives us the right to keep ourselves alive through perpetual dependence on tubes and machines? How does one factor in a Natural God within an artificial, medicalized environment?
I think of Ramón Sampedro Cameán, a 25-year-old Spanish fisherman and writer who sustained spinal cord injury following a diving accident that left him paralyzed from the neck down. For the next 29 years, he fought for his right to assisted suicide. His poignant story is told in the 2004 film Mar Adentro (The Sea Inside).
I think of Sue Rodriguez who, while suffering from the debilitating effects of amyotrophic lateral sclerosis (ALS), went all the way to the Supreme Court of Canada to fight for her legal right to assisted suicide. She lost the battle in 1993 after which she took her own life with the help of an anonymous physician. In contrast, Gloria Taylor, also suffering from ALS, fought for her right to die. In her case, the BC Supreme Court ruled that the right to die with dignity is protected by the Charter of Rights and Freedoms. Taylor was allowed a special exemption, but before she could exert that right, she died in 2012 as a result of infection from a perforated colon.
………………………….
I think of Louise and me – the two of us, fifteen or twenty years from now, possibly trying like Alice in Lisa Genoa’s book (Still Alice) to find innovative ways to control our death with dignity, while at the same struggling with legal barriers that would continue to exist if the Criminal Code is not amended.
I look for a flicker of Lawrence’s “little sanity,” and I find it in the following paragraph from the 2015 Supreme Court Ruling on Physician-Assisted Suicide:
“It is a crime in Canada to assist another person in ending her own life. As a result, people who are grievously and irremediably ill cannot seek a physician’s assistance in dying and may be condemned to a life of severe and intolerable suffering. A person facing this prospect has two options: she can take her own life prematurely, often by violent or dangerous means, or she can suffer until she dies from natural causes. The choice is cruel.” (Introduction I)
The recognition that this is a “cruel” choice is a relief. The recommended amendments in legislation need to happen sooner rather than later. However, it is reassuring that the Supreme Court has given Canada a directive to address this issue and to move toward changing the Criminal Code to ensure, as far as possible, the mitigation of cruelty while having to make that one last decision.







This is a thoughtful article on a very difficult subject. I agree with the author regarding the urgency of addressing the issues raised in the article . That is a caring, responsible and humane thing to do.
Very informative and researched article. Makes a strong case for updating the Criminal Code to allow choices to terminally ill in how to end their life so as to alleviate pain and suffering.
Why do we NOT allow our pets to suffer, yet we allow our mothers, fathers, brothers, sisters, friends, uncles, aunts, friends and other people to lie suffering uncontrollably at times without help, without aid? Why do we allow this anguish? It is cruelty in the extreme.